Alternative: exposure to radiation or let the cancer evolve…
For over 20 years, there has been a steady increase in the survival of patients treated for cancer. This improvement, which affects some of the most common cancers like breast cancer and colorectal cancer, is due both to advances in treatment and in testing. Today, 2 to 3% of people living in Europe have had cancer, treated more than 2 years ago and have been healed. In France, these survivors are now more than a million. Radiation therapy is part of their treatment in more than half of cases.
Radiotherapy and chemotherapy being at the origin of these advances have carcinogenic effects, which may cause second cancer years later. These effects are explained by the mode of action of these therapies that are only effective against the tumor because of their toxicity. There is no model to predict the long-term toxicity.
Therefore, the question is asked about secondary cancers potentially induced by radiation therapy. Although progress has been made with the use of electrons and heavier particles as well as brachytherapy, today no technique may restrict irradiation just to tumor tissues.
For example, a study of 7711 women treated for breast cancer showed that they had received an average dose of 9 Gy (Gray) to the thyroid. Iodine-131 used for cancers of the same thyroid delivers doses of significant radiation to the bone marrow, bladder and digestive system.
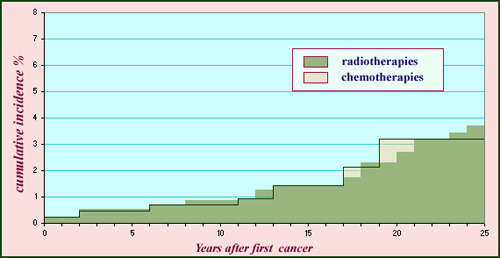
Childhood cancer: risk of radiotherapies
The cumulative incidence is the rate of cancer that occurred after treatment of a first cancer. The histogram shows the impacts in terms of years for a cohort of 4500 children who had been treated for cancer by chemotherapy or radiotherapy between 1943 and 1985. Over 25 years, the incidence of a second cancer approaches 4% for radiotherapy and chemotherapy. It is estimated that during 30 years after treatment, children treated with radiotherapy are subject to a risk 5 to 10 times higher than children who did not undergo a first cancer.
© IN2P3
It is primarily for children, being still growing and therefore more sensitive to radiation, that the risk is important. In a sample of children treated with radiation for solid cancer and followed thereafter over a long period, there was an increased likelihood of a second cancer long after.
However this danger, similar to that incurred by chemotherapy, must be compared with years of life that these children would not have had if their first cancer had not been treated.
The risk exists and should not be concealed: many sets of patients were studied and the corresponding epidemiological statistics published. This work continues and is followed closely by oncologists and radiation therapists. But waiting for the hypothetical advent of new anti-cancer technologies, we should accept a long-term risk rather minimal compared to a positive result almost certain in the short term. Take the case of a patient where the existence of a rapidly developing tumor is suspected, inaccessible to surgery and likely to hit its vital functions within weeks to months. If we can, by techniques using radiation (radiography, scintigraphy, radiotherapy) locate and destroy the cancer, we know in advance that we will primarily save his life, but also weaken his body a bit and perhaps even induce a risk of developing a second cancer, radiation-induced, for which the development period is counted in years or even decades. And, we repeat, this is an eventuality that has a relatively low statistical chance to occur.
Under these conditions, it is obviously the physician or physician group that has supported the patient, who faces up his responsibility to initiate a particular action that will respect the principle of maximum profit, thanks to a strategy adapted to each case. But between an immediate fatal risk and a possible risk in the very long term, there is no room for hesitation.
Other articles on the subject « Radiation Therapy »
Radiotherapies
X-rays but no radioactivity Radiotherapy today denotes all cancer treatments based on ionizing ra[...]
Metabolic Therapies
Therapeutic Radioisotopes Applications of radioisotopes in nuclear medicine are not limited to sc[...]
Brachytherapies
The oldest nuclear therapy modernized today Brachytherapies (or Curietherapies) are the oldest th[...]
Prostate Brachytherapy
An Efficient destruction of cancerous cells Since the 2000s, particularly in the United States an[...]
Protontherapies
Proton therapy: an advanced and precise radiotherapy Proton therapy involves treating tumors with[...]